Since 2019, dengue has appeared with a very atypical presentation. From 2021, the main focus of dengue is on plasma leakage which abruptly reduces organ perfusion following hypovolemia and severe lactic acidosis, and extreme cellular dehydration.
A common idea has arisen among us that in dengue, there will be high fever, severe body pain, body rash, and platelet will decrease slowly. But nowadays in dengue, the platelets are decreasing suddenly, patients are responding slowly even after being given plasma apheresis.
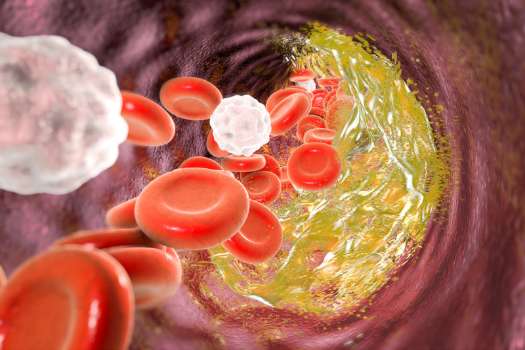
There is micro vasculature leakage within the body, we are unnoticed.
I would like to say to medical colleagues – put the main focus on blood pressure. Remember, you will not get the clinician feature of hypovolemic shock unless there is 30-40% fluid loss. So, a decrease in BP means- the pt has already lost his 30-40% fluid volume. So, we should Monitor BP intimately. If the diastolic BP is elevated, assume the patient’s pulse pressure is narrowing. A minimum of 60-70 mm MAP (Mean Arterial Pressure) is required for each organ perfusion. Decreased pulse pressure is an early sign of shock!
Please check LFT, and CRP after fever, these reports will give you advanced idea about shock liver. Get serum creatinine and Renal Profile done. (Please follow dengue national guidelines). Progressive shock or established shock will require colloid +/- inotropes following resus fluid. The patient will take fluids per mouth as long as he can and should add Vitamin C which is very effective as an antioxidant.
Please take care of the patient’s urine output. Mark the bottle and ask the patient to urinate there. The minimum output should be 1ml/kg/hour. Some patients are presenting with gastroenteritis. If a patient has abdominal pain, USG of the whole abdomen should be advised. Physicians should auscultate the base of the lungs, breathing exercises in mandatory. Check whether the patient’s breathing or oxygen demand is increasing. Do not hesitate to send Trop I if there are chest pains or the ECG shows nonspecific changes, should exclude DENGUE MYOCARDITIS and should not prescribe any Anti platelet without confirming Dengue Antibody.

You have to take care of Hb count or PCV in CBC (If it increases, you will understand that the patient is hemoconcentration due to cellular dehydration! Resus and maintenance fluid should be given to the patient according to the guidelines.
Be careful with viral myocarditis/pericarditis. Avoid NSAIDS and antiplatelets.
If dengue NS1 and IgG, IgM -ve found, chikungunya RT PCR should be done. Both dengue and chikungunya are transmitted by Aedes.
But we are not sure yet – whether Dengue and Chikungunya exchanged genetic codes, genomes and gave rise to stronger strains!
Whether dengue has developed a new anti-platelet antibody and has the ability to not respond to platelet apheresis!
Contents
Conlusion:
Dengue fever has been turning heads with some unexpected changes since 2019. Now, it’s all about plasma leakage, low fluid levels, and some tricky platelet behavior that’s making diagnosis and treatment a bit of a puzzle. It’s not following the usual script, you see – platelets are dropping suddenly, and patients aren’t bouncing back as quickly after getting plasma treatment.
There’s this microvascular leakage happening inside the body that often goes unnoticed, but it’s a big deal in how Dengue works. Doctors need to keep a close eye on blood pressure because a drop there could mean the patient has lost a lot of fluids already.
Tests like LFT, CRP, and checking certain levels are super important to catch any signs of shock early. Treating Dengue now involves some extra steps like using specific fluids, being careful with medications, and keeping a check on vitamin levels.
What’s interesting is this possibility that Dengue and Chikungunya might be sharing some genetic stuff, making things more complicated. So, being cautious with medications and doing more precise tests when Dengue tests aren’t clear is a must.
Dr. Asif-Ur-Rahman knows their stuff. With loads of experience and being a member of The Royal College of Emergency Medicine – RCEM UK, they’re bringing some solid insights and recommendations based on practical experience.
In a nutshell, Dengue’s changing, and we need to adapt. It’s about being more aware, following new protocols, and making sure we’re on top of things to give patients the best shot at beating this tricky infectious disease.
Read more
| 1.The Benefits of Membership in the Royal College of Emergency Medicine | Link 1 |
| 2. Dengue Myocarditis | Link 2 |
| 3. A Comprehensive Guide for Success in MRCEM OSCE | Link 3 |
| 4. How to Open an RCEM Account | Link 4 |
| 5. How to Take a Core Preparation for MRCEM-UK | Link 5 |
| 6. Accident & Emergency Medicine UK: Decoding the Crucial First Response | Link 6 |

Excellent
The provided content highlights the evolving nature of dengue presentation since 2019, specifically focusing on plasma leakage and shock. The author emphasizes the criticality of monitoring blood pressure as a crucial indicator of fluid loss and the progression of shock. They suggest closely observing various parameters such as platelet count, liver function tests, C-reactive protein, serum creatinine, and renal profile to evaluate organ involvement and anticipate the onset of shock. The importance of monitoring urine output, recognizing abdominal pain, and being vigilant about respiratory symptoms is also emphasized. Additionally, the author advises against the prescription of antiplatelets without confirming dengue antibodies, cautioning against the use of NSAIDs and antiplatelets due to the potential risks of viral myocarditis/pericarditis. The content raises the possibility of Dengue and Chikungunya strains interchanging genetic codes, potentially leading to the emergence of more potent strains. Concerns are also expressed about the development of new anti-platelet antibodies that may not respond to platelet apheresis. The author concludes by sharing their professional credentials and affiliation. Thank you for sharing this informative content.
Thanks a lot.
Well said!!!
Great!!